### The AI Undercurrent: Decoding the Real Signals in Recent Med-Tech Moves
The med-tech news cycle is a relentless torrent of funding rounds, partnerships, and preclinical data announcements. It’s easy to see these as isolated events—a capital injection here, a strategic alliance there. But for those of us tracking the deep currents of artificial intelligence in healthcare, these are more than just headlines. They are data points that, when connected, reveal the architecture of a new, intelligent paradigm in medicine. A recent flurry of activity involving firms like Tempus AI, Renalytix, and Argá Medtech isn’t just noise; it’s a clear signal of where the smart money and smarter technology are headed.
Let’s dissect these developments to understand the underlying AI strategy at play.
—
### The Data Moat: The Unseen Engine of Precision Medicine
At the heart of the modern med-tech revolution isn’t just the algorithm, but the data that fuels it. Look no further than **Tempus AI**, a company whose entire business model is built on creating one of the world’s largest libraries of clinical and molecular data. When a giant like **Roche** engages with or operates in the same ecosystem as a data-centric player like Tempus, it’s not just about a single product. It’s a strategic move to access a “data moat”—a proprietary, high-quality dataset so vast and well-structured that it becomes a formidable competitive advantage.
The real technical challenge Tempus solves isn’t just data storage; it’s data *harmonization*. They integrate unstructured data from physician notes, structured data from electronic health records (EHRs), genomic and transcriptomic data, and pathology images into a single, queryable resource. This multi-modal approach is critical. An AI model trained only on genomic data might identify a mutation, but a model trained on a Tempus-style dataset can correlate that mutation with treatment responses, clinical trial outcomes, and real-world evidence. This is the foundation of true personalization, moving beyond one-size-fits-all therapies to dynamically informed clinical decisions.
### From Prediction to Personalization: AI in the Clinic
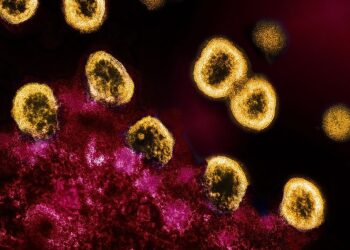
While large-scale data platforms provide the fuel, companies like **Renalytix** are building the high-performance engines for specific clinical applications. Their work in kidney health is a masterclass in deploying predictive analytics. The *KidneyIntelX* platform doesn’t just analyze a single biomarker; it integrates blood-based biomarkers with a patient’s EHR data, using a machine learning algorithm to generate a highly accurate risk score for progressive kidney disease.
This represents a critical shift from reactive to proactive care. The AI isn’t just identifying patients who are already sick; it’s flagging those at high risk of rapid decline, allowing clinicians to intervene *before* irreversible damage occurs. This is the promise of AI in diagnostics: augmenting clinical judgment with a probabilistic forecast, enabling earlier, more targeted interventions. Similarly, firms like **True-See**, which focus on wound care imaging, leverage computer vision models to objectively assess healing, track progress, and detect signs of infection far more consistently than the human eye alone. It’s about turning subjective observation into quantifiable data.
### Intelligent Intervention: Fusing AI with Medical Hardware
AI’s influence isn’t confined to software and diagnostics. It is increasingly being embedded directly into therapeutic devices. Consider a company like **Argá Medtech**, which operates in the cardiac ablation space. Conventional ablation procedures for conditions like atrial fibrillation rely heavily on the skill and experience of the electrophysiologist.
The next generation of these devices, however, will be AI-driven. Imagine a system that uses AI to:
1. **Process real-time signals** from heart tissue to differentiate healthy from diseased cells with superhuman accuracy.
2. **Create dynamic 3D maps** of the heart’s electrical activity, pinpointing the precise sources of arrhythmia.
3. **Guide the ablation catheter** and modulate energy delivery to create effective, lasting lesions without damaging surrounding tissue.
This is the fusion of robotics, signal processing, and machine learning. The AI doesn’t replace the physician; it equips them with an intelligent co-pilot, turning a complex manual procedure into a precise, data-driven intervention. The investments flowing into this space from venture firms like **T Rx Capital** signal a strong belief that the future of medical devices is inseparable from the intelligence they contain.
—
### Conclusion: An Interconnected, Intelligent Future
These recent happenings are not disparate events. They are interconnected nodes in a rapidly evolving ecosystem. The data platforms built by companies like Tempus provide the foundational layer. The diagnostic and predictive tools from Renalytix and others build upon this foundation to identify risk and guide clinical decisions. Finally, the intelligent hardware from innovators like Argá Medtech executes the therapeutic intervention with unprecedented precision.
The narrative is clear: we are moving beyond siloed “AI projects” and toward an integrated, intelligent healthcare infrastructure. The technical hurdles of data quality, model validation, and regulatory approval remain significant, but the trajectory is undeniable. The real revolution isn’t a single algorithm; it’s the network effect of combining data, diagnostics, and delivery into a seamless, learning system that promises a more predictive, personalized, and effective standard of care.
This post is based on the original article at https://www.bioworld.com/articles/724126-other-news-to-note-for-sept-19-2025.