### Beyond the Brain Scan: AI’s Algorithmic Shift in Early Alzheimer’s Detection
For decades, the fight against Alzheimer’s disease has been a frustratingly reactive one. Diagnosis has often relied on the emergence of clinical symptoms, supported by costly and invasive procedures like PET scans or cerebrospinal fluid analysis. By that point, significant and often irreversible neurodegeneration has already occurred. The consensus in the field is clear: to truly change outcomes, we must move from diagnosis to prognosis. The key lies in identifying the disease at its most nascent, preclinical stages.
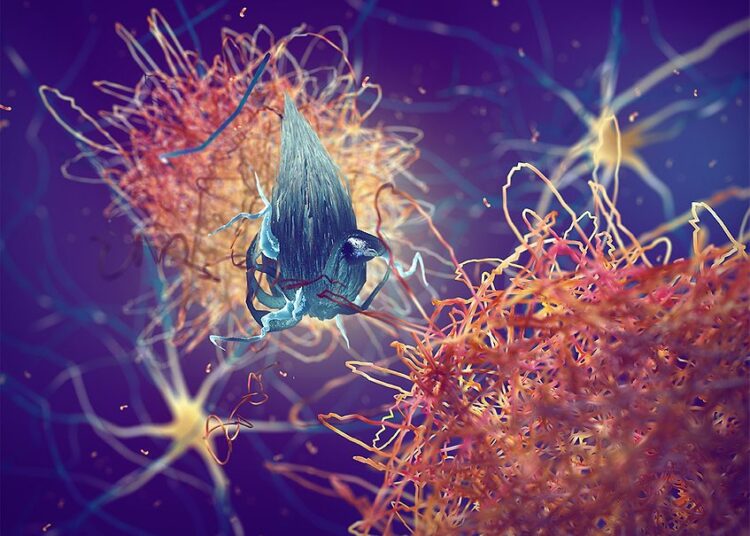
This is where the paradigm is shifting, driven by the convergence of two powerful forces: blood-based biomarkers and artificial intelligence. The ability to detect subtle molecular signals of Alzheimer’s pathology in a simple blood sample represents a monumental leap forward. But these signals are not a single, glaring red light; they are a complex, faint symphony of data. This is where AI becomes not just a tool, but an indispensable partner.
—
#### The Challenge: From a Single Snapshot to a High-Dimensional Portrait
Traditional diagnostic methods often look for one or two key indicators, like the presence of amyloid plaques. The new frontier, however, involves building a comprehensive, multi-modal profile of each individual. This isn’t a single data point; it’s a high-dimensional data portrait composed of:
* **Genomics:** Analyzing genetic risk factors like the APOE ε4 allele and other single-nucleotide polymorphisms (SNPs).
* **Proteomics:** Quantifying levels of specific proteins in the blood, such as phosphorylated tau (p-tau217) and amyloid-beta 42/40 ratios, which are direct reflections of the disease’s core pathology.
* **Immunology:** Measuring inflammatory markers and cytokines, as neuroinflammation is now understood to be a critical component of Alzheimer’s progression.
* **Clinical Data:** Integrating longitudinal data from electronic health records, including cognitive scores, lifestyle factors, and comorbidities.
No human clinician, however brilliant, can manually synthesize these disparate, noisy datasets and extract a clear, predictive signal. The patterns are too subtle, the interdependencies too complex. A slight elevation in one inflammatory marker might be insignificant on its own, but when combined with a specific genetic profile and a borderline p-tau level, it could represent a powerful early warning sign.
#### Machine Learning: The Engine of Discovery
This is a classic high-dimensional pattern recognition problem, and it’s precisely what machine learning (ML) models are built for. Instead of relying on predefined thresholds, we can train sophisticated algorithms on vast datasets from thousands of patients, allowing them to *learn* the complex signature of preclinical Alzheimer’s.
Here’s how it works in practice:
1. **Feature Engineering and Selection:** AI models can sift through hundreds or even thousands of potential biomarkers to identify the most predictive combination. This helps focus future research and development on the markers that truly matter.
2. **Classification and Risk Stratification:** We employ models like Gradient Boosting Machines or Deep Neural Networks to analyze a patient’s complete profile. The output isn’t a simple “yes” or “no.” Instead, the model generates a probabilistic risk score—for example, a “75% probability of developing mild cognitive impairment within the next five years.” This allows clinicians to stratify patients and prioritize those who would benefit most from early intervention.
3. **Personalized Subtyping:** Alzheimer’s is not a monolith. AI is helping us uncover disease subtypes based on the dominant underlying biology. One patient’s risk profile might be heavily driven by amyloid dysregulation, while another’s might be characterized by a strong neuroinflammatory signature. This is the cornerstone of personalized medicine. An intervention targeting inflammation may be highly effective for the second patient but useless for the first. AI provides the map to guide these targeted therapeutic strategies.
—
#### The Road Ahead
The integration of AI into the analysis of blood-based biomarkers is fundamentally changing our approach to Alzheimer’s disease. We are moving away from a one-size-fits-all, late-stage diagnostic model to an early, precise, and personalized framework for risk assessment and prevention.
The challenges ahead involve standardizing data collection across diverse populations, ensuring model fairness and interpretability, and seamlessly integrating these AI-powered tools into clinical workflows. However, the trajectory is clear. By leveraging AI to decode the complex language of our own biology, we are poised to finally shift the battle against Alzheimer’s from a defensive reaction to a proactive, preemptive strategy, giving millions of people a chance to rewrite their future.
This post is based on the original article at https://www.bioworld.com/articles/724570-ptau217-could-change-how-alzheimers-is-diagnosed.