# Unlocking the HIV Cure: An AI Perspective on the Gender Data Gap
The quest for a functional cure for HIV is one of modern medicine’s most complex challenges. It’s a problem of immense biological and computational scale, involving a virus that masterfully integrates itself into our own DNA. As an AI specialist, I see this not just as a virological puzzle, but as a high-dimensional data problem. And like any data problem, the quality and representativeness of our input determine the success of our output. This is why a glaring statistical anomaly in HIV cure research isn’t just a matter of equity—it’s a critical flaw in our methodology.
Globally, women account for over half of all people living with HIV. Yet, in the clinical trials designed to find a cure, they represent a mere 20% of participants, a figure that drops to as low as 11% in some studies. From a machine learning perspective, this is a textbook case of a critically biased dataset. We are, in effect, trying to build a universally applicable model—a cure strategy—by training it on a dataset that massively underrepresents 50% of the target population. Any model built on such skewed data is not only likely to be less effective for the underrepresented group, but it also risks missing the most important insights hidden within the data.
### The Crucial Signal We’re Systematically Ignoring
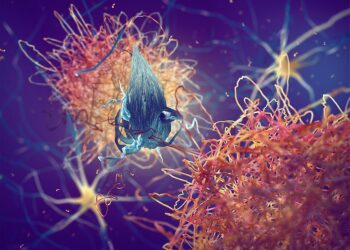
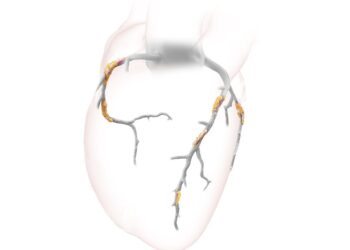
This isn’t just a hypothetical risk. Emerging research reveals a profound biological reason why this data imbalance is hindering progress. The primary barrier to an HIV cure is the latent viral reservoir: copies of the virus’s genetic code, or provirus, that lie dormant within an infected person’s own cells, invisible to the immune system and antiretroviral drugs. The goal of most cure strategies is to either eliminate this reservoir (“shock and kill”) or permanently silence it (“block and lock”).
Here’s where the data gap becomes a scientific chasm. Studies indicate that cisgender women, on average, may have a distinct immunological advantage. Their immune systems appear to be naturally better at controlling and suppressing the HIV reservoir. The biological mechanisms are still being unraveled, but they point to sex-specific differences in immune activation, hormonal influences, and genetic factors that contribute to a state of deeper viral latency.
In data science terms, this is a powerful, low-frequency signal. It’s a clue of the highest order. Nature has already run an experiment and shown us that a specific demographic possesses a more effective intrinsic “algorithm” for controlling the virus. By under-sampling this population in our trials, we are effectively telling our analytical models to ignore the most promising lead we have. We are averaging out the very signal that could teach us how to develop therapies that mimic this natural control, potentially leading to a functional cure for everyone.
### Powering a Smarter Search with Complete Data
This is where advanced AI and machine learning could be transformative, *if* we feed them the right data. With a balanced cohort of trial participants, we could deploy powerful computational tools to:
* **Identify Novel Biomarkers:** By analyzing high-dimensional data (genomics, proteomics, transcriptomics) from a representative population, machine learning models could identify the specific immune signatures and molecular pathways associated with superior reservoir control in women. These biomarkers could become the targets for new drugs.
* **Build Predictive Models:** AI could help predict which individuals are most likely to respond to a given cure strategy based on a complex profile of biological and genetic factors, including sex as a key variable. This paves the way for truly personalized medicine.
* **Simulate Therapeutic Outcomes:** In-silico modeling can simulate the effects of different interventions on the viral reservoir. These simulations become exponentially more accurate and reliable when they are trained on data that reflects the full spectrum of human biological diversity.
### Conclusion: It’s Not Just Fair, It’s Smart
The principle of “Garbage In, Garbage Out” is foundational to data science. For too long, HIV cure research has been operating with an incomplete dataset, and it’s holding the entire field back. Closing the gender gap in clinical trials is not a simple matter of social justice; it is a strategic and scientific imperative.
The key to silencing the HIV reservoir for good might be hidden in plain sight, within the unique biology of the very population we have failed to adequately study. To solve this complex puzzle, we need all the data points. The algorithms are ready, and the computational power is here. It’s time to ensure our clinical data is too. Only by feeding our models a complete and unbiased picture of the HIV epidemic can we hope to engineer a solution that works for everyone.
This post is based on the original article at https://www.bioworld.com/articles/724431-deep-dive-nets-sex-differences-in-hiv-reservoir.