### From Pixels to Plaque: Why Heartflow’s Latest Milestone is a Watershed Moment for Medical AI
In the world of artificial intelligence, we often talk about breakthroughs in abstract terms—better benchmarks, novel architectures, more efficient training. But every so often, a development comes along that grounds the abstraction in the tangible, life-saving reality of clinical practice. Heartflow Inc.’s recent dual announcement—FDA 510(k) clearance for its next-generation plaque analysis platform and comprehensive Cigna coverage—is precisely one of those moments.
As technologists, it’s easy to get lost in the numbers, but the headline figure here is a critical one: the new algorithm boasts a **21% improvement in plaque detection** compared to its predecessor. This isn’t a minor tweak. This is a significant leap in a mission-critical application, and it signals a maturation of AI in one of medicine’s most complex domains.
Let’s break down why this is more than just an incremental update.
—
### The Technical Leap: Beyond a Simple Model Refresh
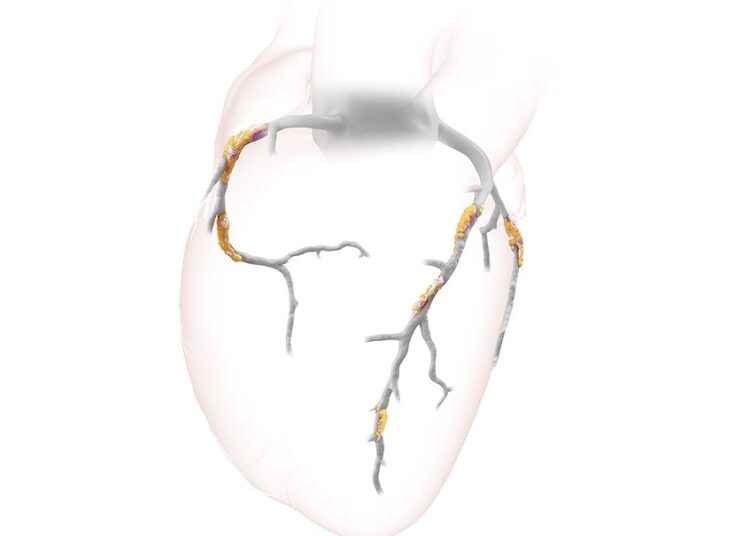
Analyzing coronary computed tomography (CT) scans for plaque is an incredibly challenging computer vision problem. We’re not just identifying cats in a photo; we’re tasked with precisely delineating and characterizing tiny, morphologically diverse deposits within a moving, three-dimensional organ. The original Heartflow Analysis was already a feat of engineering, translating 2D CT slices into a 3D model of coronary blood flow.
A 21% improvement suggests this new platform isn’t merely the result of feeding the old model more data. It points to a fundamental evolution in the underlying technology. This could involve several key advancements:
* **More Sophisticated Architectures:** We are likely seeing the deployment of more advanced convolutional neural network (CNN) architectures. Techniques like attention mechanisms, which allow the model to focus on the most salient regions of an image, or generative adversarial networks (GANs) for data augmentation and refinement, can dramatically improve the detection of subtle or atypical plaque formations that earlier models might have missed.
* **Semantic Segmentation at Scale:** The task here is precise semantic segmentation—classifying every single voxel in the scan as artery, plaque, or surrounding tissue. The improvement implies a much higher fidelity in this segmentation, allowing for not just *detection* but also more accurate *quantification* of plaque volume and characterization of its components (e.g., calcified vs. non-calcified). This granular detail is clinically paramount for risk stratification.
* **Robustness and Generalization:** A key hurdle for medical AI is generalizing across different patient populations, scanner models, and imaging protocols. A significant performance jump often indicates that the model has been trained on a far more diverse and rigorously annotated dataset, making it more reliable in real-world clinical settings, not just in a sanitized lab environment.
This technical progress is the engine driving the clinical value. It translates directly to a more confident, accurate, and non-invasive diagnosis for patients with suspected coronary artery disease (CAD).
### The Trust Flywheel: Regulatory and Commercial Validation
For any AI system in healthcare, technical prowess is only half the battle. The other half is trust. This is where the dual announcement becomes so powerful.
1. **FDA 510(k) Clearance:** This is the industry’s gold standard for demonstrating that a medical device (including software) is safe and effective. For an AI algorithm, it’s a rigorous validation process that scrutinizes everything from the training data to the model’s performance against established clinical benchmarks. Securing this clearance for a next-gen product builds a powerful layer of trust with clinicians and hospital systems. It certifies that the 21% improvement isn’t just a marketing claim—it’s a clinically validated reality.
2. **Cigna Coverage:** This is, arguably, the ultimate vote of confidence. Payor coverage transforms a technology from a promising innovation into a sustainable, accessible standard of care. Cigna’s decision to cover the analysis across all its lines indicates that the technology has demonstrated not only clinical efficacy but also economic value. It shows that non-invasively assessing plaque with this level of accuracy can lead to better patient outcomes and potentially lower healthcare costs by avoiding unnecessary invasive procedures.
This combination creates a “trust flywheel”: FDA clearance validates the science, which encourages payor coverage, which drives wider clinical adoption. Wider adoption generates more real-world data, which in turn fuels the development of even more accurate and powerful algorithms.
—
### Conclusion: From Analysis to Prediction
Heartflow’s achievement is a case study in how to successfully bring advanced AI from the research lab to the clinical front lines. It demonstrates a mastery of the entire value chain: cutting-edge computer vision, rigorous clinical validation, regulatory navigation, and successful commercialization.
The trajectory here is clear. The first step was modeling blood flow. The current step is perfecting the analysis of the underlying disease—the plaque itself. The next frontier will be **prognosis**. By analyzing the specific composition, location, and morphology of plaque, future AI models will not just diagnose current blockages but predict the likelihood of future adverse events like a heart attack.
This is where the true power of AI in medicine lies: shifting the paradigm from reactive treatment to proactive, personalized prevention. Heartflow’s latest news isn’t just a win for one company; it’s a clear signal that the future of data-driven, predictive cardiology is arriving faster than we think.
This post is based on the original article at https://www.bioworld.com/articles/724223-fda-clears-heartflows-next-gen-plaque-analysis.