# Beyond the Beltway: Why a New Medicare Bill is a Game-Changer for Medical AI
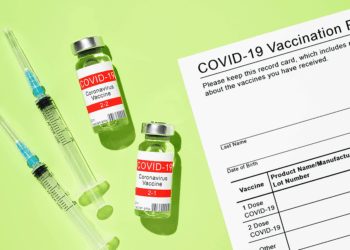
On the surface, a bill advancing through a House of Representatives committee might seem like just another piece of legislative minutiae. The bill in question, which would grant four years of Medicare coverage to FDA-designated “breakthrough” medical devices, is easy to frame as a simple healthcare policy adjustment. But for those of us working on the front lines of artificial intelligence and machine learning, this development is far more significant. It represents a potential inflection point, a policy change that could fundamentally accelerate the deployment and iteration of AI in clinical settings.
This isn’t just about funding; it’s about creating the essential infrastructure for innovation in the 21st century.
—
### The Reimbursement Chasm and the Data Flywheel
For years, the medical AI space has faced a daunting challenge that I call the “reimbursement chasm.” An innovator can spend years developing a revolutionary diagnostic algorithm—one that spots early-stage cancer in a CT scan with superhuman accuracy, for instance. They can navigate the rigorous, multi-year process of securing FDA approval. But even with that regulatory green light, they hit a wall: getting paid. Without a clear path to reimbursement from major payors like Medicare, a groundbreaking device can wither on the vine, trapped in a commercial valley of death. Hospitals are hesitant to adopt technology they can’t bill for, and patient access remains severely limited.
This bill, if passed, provides a crucial four-year bridge across that chasm. It gives innovators a predictable window of market access, transforming the economic calculus for R&D and venture investment. But the implications run deeper than just the business case. The most powerful effect of this legislation would be the creation of a massive, real-world data flywheel.
AI models, particularly in healthcare, thrive on data. The models we train in sterile, curated datasets are only a starting point. True algorithmic efficacy and robustness are forged in the crucible of real-world clinical practice, with all its messy, diverse, and unpredictable variables. Four years of guaranteed Medicare coverage means that instead of being used in a handful of elite research hospitals, these AI-powered devices will be deployed across a wide spectrum of patient populations and clinical environments.
This triggers a virtuous cycle:
1. **Wider Adoption:** Medicare coverage drives adoption in diverse healthcare settings.
2. **Massive Data Inflow:** Each use of the device generates valuable real-world performance data.
3. **Model Refinement:** Developers can use this data (with appropriate privacy safeguards) to identify edge cases, mitigate algorithmic bias, and improve model accuracy and generalizability.
4. **Improved Outcomes:** The refined algorithm delivers better, more equitable patient outcomes, further justifying its use and driving even wider adoption.
This flywheel is the engine of iterative improvement that has defined the tech industry, and this bill effectively provides the fuel to get it started in medicine.
### De-Risking a New Class of Device
It’s also critical to understand what “breakthrough device” means in 2024. Increasingly, it doesn’t refer to a new titanium alloy or a novel surgical tool. The breakthrough element is the software, the algorithm, the “ghost in the machine.” We’re talking about Software as a Medical Device (SaMD), from predictive analytics platforms that forecast sepsis risk in ICUs to AI-powered tools that help plan complex radiation oncology treatments.
Traditional reimbursement pathways were designed for static hardware, not for dynamic, learning software. This bill implicitly acknowledges that the nature of medical innovation has changed. By providing a clear, temporary pathway to payment, it de-risks the entire category of AI-driven medical technology. It sends a powerful signal to the market that a viable commercial path exists for a new class of device defined not by its physical form, but by its intelligence.
—
### The Path Forward
Of course, challenges remain. The industry and regulators will need to develop robust frameworks for post-market surveillance and for managing the lifecycle of continuously learning algorithms. How do we handle a device whose core model is updated every six months? How do we ensure that the real-world data being collected is used to actively reduce bias rather than amplify it?
These are not trivial questions. But they are the *right* questions to be asking. This proposed legislation doesn’t solve them, but it moves the entire field onto the playing field where we can begin to tackle them at scale. It’s a pragmatic and powerful step toward closing the gap between what is technically possible in medical AI and what is actually available to patients. This isn’t just a healthcare bill; it’s a piece of foundational technology policy.
This post is based on the original article at https://www.bioworld.com/articles/724132-house-committee-advances-medicare-breakthrough-devices-coverage-bill.