### The Ghost in the Machine: How AI Is Decoding Neuronal Sabotage in Lung Cancer
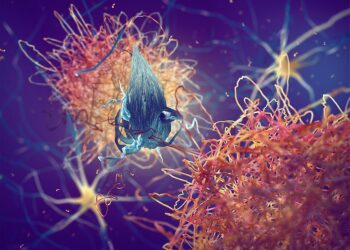
The tumor microenvironment (TME) has long been understood as a complex battlefield, a chaotic interplay of cancer cells, immune infiltrates, and stromal components. For decades, our models of this environment largely overlooked one of its most fundamental components: the nervous system. We treated neurons as passive wiring, the ghost in the machine. That view is now being radically revised, and two landmark papers published back-to-back in this month’s *Nature* (September 10, 2025) illuminate not only the critical role of neurons in cancer progression but also the indispensable role of artificial intelligence in making these discoveries possible.
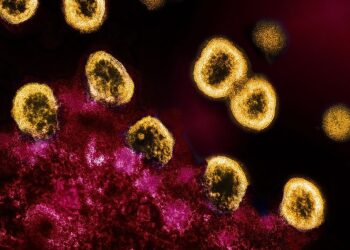
The papers focus on small-cell lung cancer (SCLC), an aggressive malignancy with notoriously poor outcomes. Building on prior work in gliomas and peripheral cancers—where nerve-tumor crosstalk is known to drive progression and blunt therapeutic response—these new studies reveal a sophisticated and insidious partnership. They demonstrate that SCLC cells don’t just co-exist with nerve fibers; they actively co-opt and remodel them to create an immunosuppressive fortress, rendering treatments like immunotherapy ineffective.
This is a biological revelation, but the story behind the discovery is a computational one. The sheer complexity of mapping these neuro-tumoral interactions across thousands of patient samples is beyond the scope of human analysis. This is where advanced AI and machine learning models became the key to unlocking this new frontier of oncology.
—
#### Main Analysis: From Pixels to Pathways
The core challenge in studying the TME is its spatial heterogeneity. A traditional bulk RNA-sequencing analysis might tell you *what* genes are expressed, but it loses the crucial information of *where*. Understanding how a neuron influences a cancer cell requires knowing their precise physical relationship.
**1. High-Throughput Phenotyping with Convolutional Neural Networks (CNNs)**
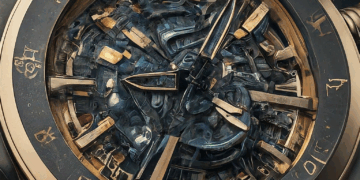
The first major hurdle was to identify and map the nerve-tumor interface at scale. The researchers leveraged high-resolution imaging of SCLC biopsies, but manually annotating axons, nerve endings, and tumor cells is impossibly slow and subjective. Instead, they trained a custom-built CNN, a U-Net architecture, to perform semantic segmentation on these images. Fed with terabytes of data, the model learned to delineate cellular and subcellular structures with superhuman accuracy and speed.
This allowed the team to quantify a new biomarker: “neuro-tumoral synapse density.” They discovered a direct, powerful correlation between a high density of these interfaces and resistance to PD-1/PD-L1 checkpoint inhibitors. The AI didn’t just see cells; it identified and quantified a previously invisible architectural pattern linked directly to patient outcomes.
**2. Modeling the Network with Graph Neural Networks (GNNs)**
Identifying the interface was just the start. The next question was: how are these cells communicating? This is not a simple one-to-one interaction; it’s a complex network of signaling. To model this, the research teams turned to Graph Neural Networks (GNNs).
They represented the TME as a graph, where each cell (tumor, neuron, T-cell, macrophage) was a node, and the edges represented potential interactions based on physical proximity and receptor-ligand expression profiles derived from spatial transcriptomics. By propagating information across this graph, the GNN could learn the complex, multi-step signaling cascades that define the system’s behavior.
The GNN model was the breakthrough. It identified a specific pathway: tumor-secreted factors were triggering nearby nerve fibers to release neuropeptides, which in turn acted on macrophages to polarize them towards an immunosuppressive M2 phenotype. This wasn’t a simple correlation; the GNN modeled a directional, causal-like chain of events that explained *how* the neurons were orchestrating immunotherapy resistance. It found the mechanism in the noise.
—
#### Conclusion: The Dawn of a Neuro-Oncologic AI
These *Nature* papers do more than just add another variable to our understanding of SCLC. They represent a paradigm shift, one powered by AI. We’ve moved from a static, cell-centric view of cancer to a dynamic, systems-level perspective where the nervous system is a key player.
The implications are profound. Computationally-derived biomarkers like “neuro-tumoral synapse density” could soon become standard for stratifying patients for immunotherapy. More excitingly, by using models like GNNs to pinpoint the exact signaling pathways at play, we can now design novel therapeutic strategies. Instead of just targeting the tumor or the immune system, we could develop drugs that sever this neuro-tumoral communication line, effectively dismantling the cancer’s defenses.
This research sits at the convergence of neurobiology, oncology, and artificial intelligence. It’s a powerful demonstration that the next great leaps in medicine won’t come from a single discipline, but from a new class of scientists and clinicians who can wield these complex computational tools to ask questions we previously didn’t even know how to formulate. The ghost in the machine is finally coming into focus, and AI is the lens making it possible.
This post is based on the original article at https://www.bioworld.com/articles/724350-rewiring-sclc-a-neural-path-to-therapy.