# The Unseen Engine: How AI is Quietly Revolutionizing Clinical Trials
The life sciences news cycle is a constant stream of clinical updates. We see headlines about trial initiations, enrollment milestones, and pivotal data readouts from companies like Biocardia, Bridge to Life, Imperative, and Masimo. On the surface, these are discrete corporate achievements. But look deeper, and you’ll see the traces of a fundamental paradigm shift. Beneath the traditional framework of clinical research, an unseen engine is running: Artificial Intelligence.
As an AI technologist, I see these announcements not just as medical progress, but as evidence of a profound operational transformation. The entire clinical trial pipeline, from hypothesis to publication, is being systematically re-engineered with machine learning. The common thread linking these disparate company updates is the drive for speed, precision, and a higher probability of success—all domains where AI excels.
Let’s break down how this is happening at each stage mentioned in these updates.
—
### Main Analysis: Deconstructing the AI-Powered Trial
#### 1. Smarter Trial Initiation and Patient Recruitment
A trial initiation isn’t just about filing paperwork; it’s the culmination of immense preclinical work and strategic planning. A major failure point is flawed trial design and, crucially, poor patient selection. This is where AI is making its first major impact.
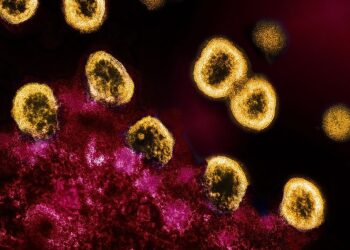
Instead of relying solely on broad inclusion/exclusion criteria, AI platforms can now sift through millions of anonymized Electronic Health Records (EHRs), genomic data, and imaging scans to build highly specific patient cohorts. Machine learning models can identify digital phenotypes—subtle patterns in patient data that correlate with disease progression or treatment response. For a company like **Biocardia**, focused on cardiac cell therapies, this means moving beyond simple metrics like ejection fraction. AI can analyze cardiac MRIs to identify specific tissue characteristics that predict which patients are most likely to benefit from their therapy, de-risking the trial from day one. This process, known as precision patient stratification, turns recruitment from a brute-force search into a targeted, data-driven exercise.
#### 2. Accelerating Enrollment and Optimizing Operations
Once a trial is underway, maintaining momentum is key. Enrollment status updates are a key performance indicator, and delays here can cost millions and postpone the availability of life-saving treatments.
AI is transforming this logistical challenge into a predictive science. Algorithms can analyze geographic, demographic, and clinical site performance data to forecast enrollment rates and identify potential bottlenecks before they occur. Furthermore, the rise of decentralized trials and wearable technology, an area where a company like **Masimo** operates, creates a deluge of real-time data. This is a perfect application for AI. Machine learning models can monitor this continuous stream of physiological data to:
* **Predict adverse events:** Identify subtle deviations in a patient’s vitals that might signal an impending issue.
* **Monitor protocol adherence:** Ensure patients are taking medication or using devices as required.
* **Identify early efficacy signals:** Detect subtle positive changes far earlier than a scheduled clinical visit.
This creates a dynamic feedback loop that keeps trials on track, reduces patient dropout rates, and provides a richer, more continuous dataset for analysis.
#### 3. Deeper Insights from Data Readouts and Publications
The final stage—data analysis and publication—has traditionally been a major time sink. A data readout is the culmination of years of work, but interpreting complex, multi-modal datasets is a monumental task.
AI is crushing this bottleneck. Where traditional statistical analysis might struggle with high-dimensional data (e.g., genomics, proteomics, and clinical outcomes), deep learning models can uncover intricate, non-linear relationships that human analysts would miss. For any company announcing a positive data readout, AI likely played a role behind the scenes, helping to:
* **Identify responder vs. non-responder signatures:** Analyze patient data to understand *why* the therapy worked for some and not others.
* **Integrate multi-modal data:** Combine imaging, biomarker, and clinical data into a single, cohesive model to get a holistic view of a drug’s effect.
* **Automate analysis pipelines:** Reduce the time from database lock to top-line results from months to weeks, or even days.
—
### Conclusion: From Incremental Updates to Exponential Progress
The clinical updates from innovators like Biocardia, Bridge to Life, and their peers are more than just milestones. They are the visible outputs of a less visible, but far more powerful, technological revolution. AI is no longer a futuristic concept in drug development; it is an integrated, foundational component of the modern clinical trial.
By embedding predictive intelligence at every step—from designing the trial to recruiting the right patients, monitoring them in real-time, and interpreting the final data—we are fundamentally changing the economics and timelines of medical innovation. The result is a more efficient, targeted, and successful R&D process. The next time you read a headline about a clinical trial update, remember the unseen engine of AI that is helping to bring tomorrow’s therapies to patients today.
This post is based on the original article at https://www.bioworld.com/articles/724115-in-the-clinic-for-sept-18-2025.